
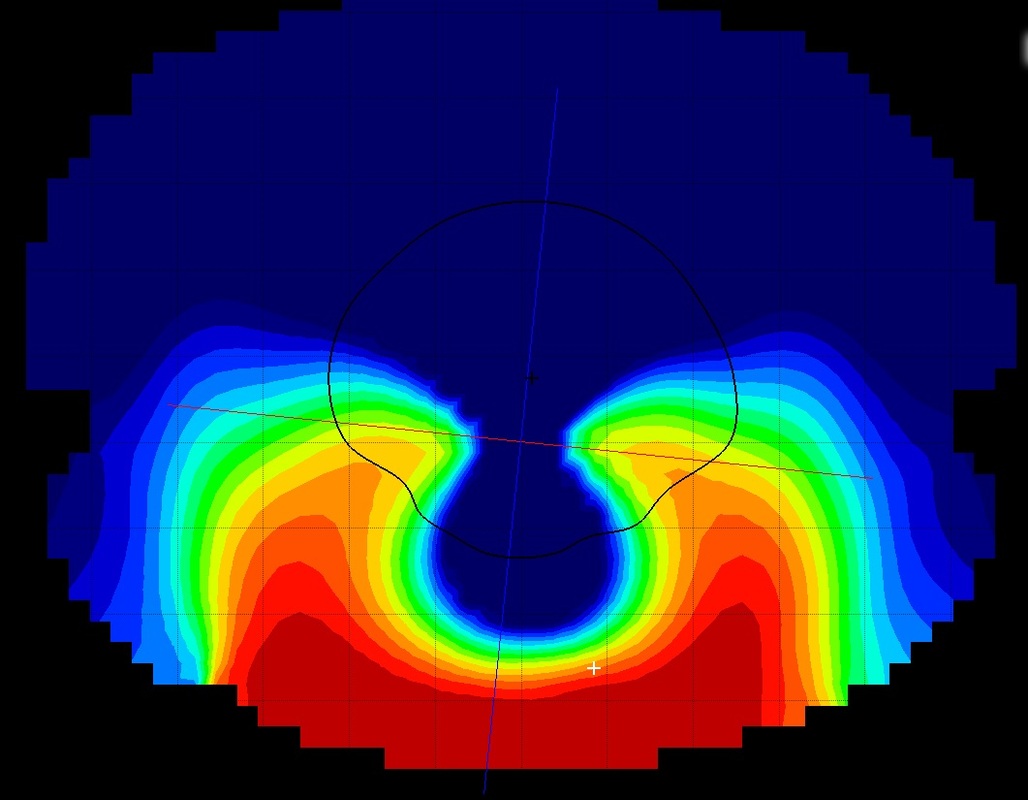
1-3 Usually, keratoconus presents in the second or third decade of life. Considered to be the most common form of ectatic disorder, primary keratoconus affects at least one out of every 2,000 members of the general population. 10 In all cases, unilateral presentation of keratoconus contraindicates surgery for the other eye because keratoconus is currently understood to be a bilateral disease. 6,8-9 Other risk factors for iatrogenic corneal ectasia include thin baseline cornea, irregular corneal thickness, high myopia (due to the need for an increased amount of ablated tissue) and young age at the time of refractive surgery. 1-6įorme fruste (i.e., subclinical) keratoconus is an often-undiagnosed latent form of biomechanical instability in the cornea, which can be induced by refractive surgery and result in post-refractive surgery ectasia. 1-6 Overall, the prevalence of post-refractive surgery ectasia is estimated to be between 0.2% and 0.66%. However, post-refractive surgery ectasia can still occur in the absence of these findings. 11,12Ĭommon clinical findings in patients with post-refractive ectasia include a thicker resulting flap or thinner residual stromal bed than expected. In two recent isolated case reports, ectasia following this procedure was documented. 1-2 Additionally, small-incision-lenticule extraction (SMILE) is a relatively novel refractive procedure that uses a femtosecond laser to remove a disc-shaped portion of stroma with no flap lift, achieving similarly successful results to those of LASIK. Iatrogenic ectasia can occur post-laser-assisted in situ keratomileusis (LASIK) or after a photorefractive keratectomy (PRK) procedure. The central caliper measure of corneal thickness is 145µm. 1īecause ectasia describes a physiological finding rather than a particular disease process, it is used in the context of various clinical entities that can arise by mechanical, degenerative or genetic factors.Īnterior chamber segment optical coherence tomography image of thin, ectatic cornea in post-LASIK ectasia.Ĭentral 9mm segment optical coherence tomography image of thin, protruding cornea in keratoglobus.

1 Corneal ectatic disorders often result in decreased acuity, increased ocular aberrations and, in some cases, the need for surgical intervention.
#KERATOCONUS VS PELLUCID MARGINAL DEGENERATION TRIAL#
Having an advanced corneal topographer and several keratoconus contact lens trial sets available in the office are a positive sign.The visual consequences of keratoconus-which has historically been defined as a noninflammatory condition with hallmark progressive corneal thinning and steepening.-can be devastating for many patients. Contact lens fitters should be selected on the basis of experience andĬommitment to aiding keratoconus patients.

Improperly fit contact lenses can cause extensive damage to the cornea and can ultimately lead to a corneal transplant. As the condition advances, specialized rigid and scleral Custom soft toric contact lenses will often provideĪdequate performance and safety. In the early stages, the central cornea is regular although highly astigmatic. We do our best to keep it simple, but our primary focus will always be on you vision and the health of your eyes.įitting patients with PMD can be especially challenging. For some patients it is a continuing process whichīegins all over again as the condition progresses. In rare cases the process can take many months. You can expect several return visits to fine-tune the fit and prescription. Fitting contact lenses on a keratoconic cornea is delicateĪnd time-consuming. The key to a successful contact lens fitting isn't as much the lens as it is the skill and experience of the contact lens fitter. Scleral lenses have rapidly become a preferred choice for many patients. Some of the newest Zen scleral lenses fitted using ultraprecise optical coherence tomography can provide exceptional comfort and outstanding vision for keratoconus Originally introduced by New Zealand Optometrist, Dr. Keratoconus and pellucid marginal degeneration. The Rose-K is an example of an exceptional and flexible corneal lens design There are numerous contact lens designs used to treat
In more advanced keratoconus, rigid gas permeable corneal or scleral contact lenses are usually the best choice for visual rehabilitation. Will often provide acceptable vision and comfort. As the disorder progresses and the corneaīecomes increasingly distorted, specially designed soft lenses ( KeraSoft IC and NovaKone), hybrid rigid-soft ( SynergEyes) lenses In the mildest form of keratoconus, eyeglasses or soft contact lenses often provide adequate vision. We are great believers in conservative treatment.


 0 kommentar(er)
0 kommentar(er)
